
TENS vs Transcutaneous Pulsed Radiofrequency: The Secret to Long-Term Pain Relief
Living with chronic pain has a profound impact on engaging in daily activities, working, sleeping – an overall change in the quality of life, usually leading to depression, anxiety and social isolation. The traditional treatment options, such as opioids and other prescription drugs, cause serious side effects, including withdrawal and addiction, and have been recognised since the 1990s as a major factor into the opioid crisis. This has led to a growing need to find drug-free, pain relief alternative therapies among which we find electrical stimulation devices that offer safe and effective managing of chronic pain, without the risk of addiction or other negative side effects.
Standard electrical stimulation devices (such as TENS) have been demonstrated to be useful tools. They are inexpensive to purchase, but thousands of studies have shown that they are only effective for short-term pain relief.
In contrast, recent evidence suggests that high frequency stimulation devices such as transcutaneous pulsed radiofrequency (TPRF) offers long-term relief for chronic pain conditions through nerve restorative (or healing) processes.
How TENS Devices Work: The Standard Square Wave
In standard therapeutic TENS devices, a square wave at frequencies ranging between 50 and 100 Hz is used for therapy. This type of stimulation pattern is slow and travels at a speed which facilitates transmembrane ionic flow – an essential and well-known mechanism for the generation of action potentials.
Despite this type of stimulating wave’s ability to generate nerve signalling, the overall therapeutic efficacy of a square wave is still under debate. Conventional TENS devices are thought to act via activation of large non-noxious nerve afferents (such as Ab sensory fibres) which, following the principle of the Gate Control Theory, prevents the transmission of painful signals from smaller nociceptive fibers (i.e., C fibers).
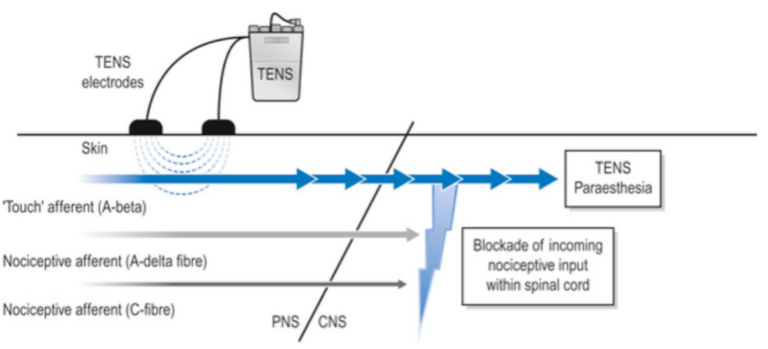
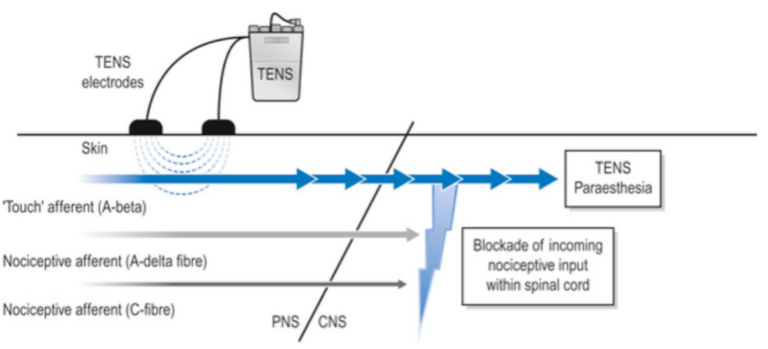
Figure 1 – Conventional TENS machine and its physiological effect on A-beta afferent fibres. According to the Gate Control Theory, when A-beta fibres are actived by TENS, nociceptive inputs from A-delta or C-fibres are blocked. Reprinted from https://musculoskeletalkey.com/transcutaneous-electrical-nerve-stimulators-for-pain-management/
The blockage of incoming painful signals is a short-term therapeutic outcome of TENS devices; however, recent animal studies have demonstrated “longer-term” effects (up to 2 hours after treatment with TENS) in releasing inhibitory neurotransmitters. This neurochemical release reduces the transmission of nociceptive inputs to the brain (i.e., hypoalgesia and pain reduction). Unfortunately, these results have yet to be reproduced on humans.
Read more about this at:
- “Transcutaneous Electrical Nerve Stimulation: Mechanisms, Clinical Application and Evidence” by M. Jonson, 2007 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4589923/
How Transcutaneous Pulsed Radiofrequency (TPRF) Devices Work: High Frequency Waves
The delivery and propagation characteristics of a high frequency waveform, like TPRF, are vastly different compared to the square waveform of standard TENS devices.
When the nerve is stimulated at radiofrequencies (above 20 kHz), the resulting electromagnetic field generates ionic vibrations, instead of the characteristic transmembrane ion flow and action potentials of TENS devices that use a square wave.
When using continuous radiofrequency stimulation, these ions will start generating heat which is the mechanism of action used in invasive radiofrequency ablation procedures, also known as rhizotomy or radiofrequency neurotomy (learn more).
When using radiofrequency for chronic pain relief, the generated energy is used differently. Instead of continuous stimulation, the TPRF waveform is pulsed and delivered as short bursts. These pulsed RF bursts are just enough to induce a small amount of energy that travels along the targeted nerve to its mitochondria.
Here, biological cascades are triggered that causes gene expression changes for a long-lasting restoration of nerve functionality. This is described by many practitioners as a reset of the nerve. For all these reasons, pulsed RF therapies not only alleviate pain symptoms but also target the underlying condition behind the pain – a vastly different therapeutic impact compared to standard TENS devices.
The Stimpod NMS460
The Stimpod NMS460 uses a proprietary hybrid radiofrequency stimulating waveform. The hybrid wave takes advantage of both components (the square wave and the high-frequency) and their two distinct modes of action.
The square wave generates an action potential which creates a fasciculation or muscle twitch, in motor nerves, and a radiating sensation for sensory nerves which is used to locate the targeted nerve.
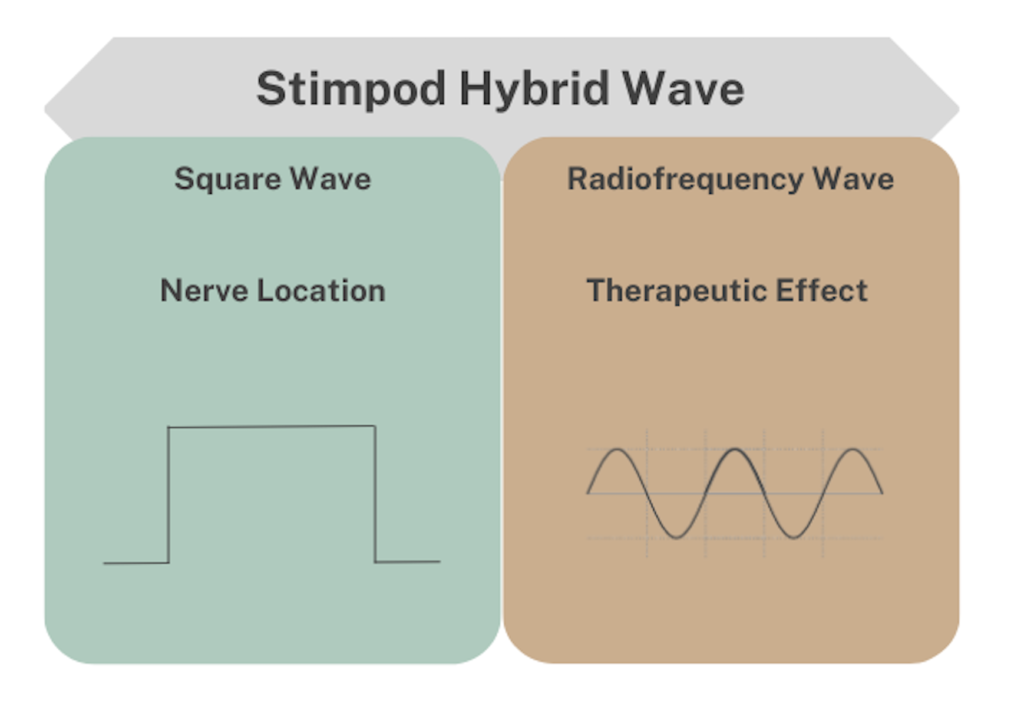
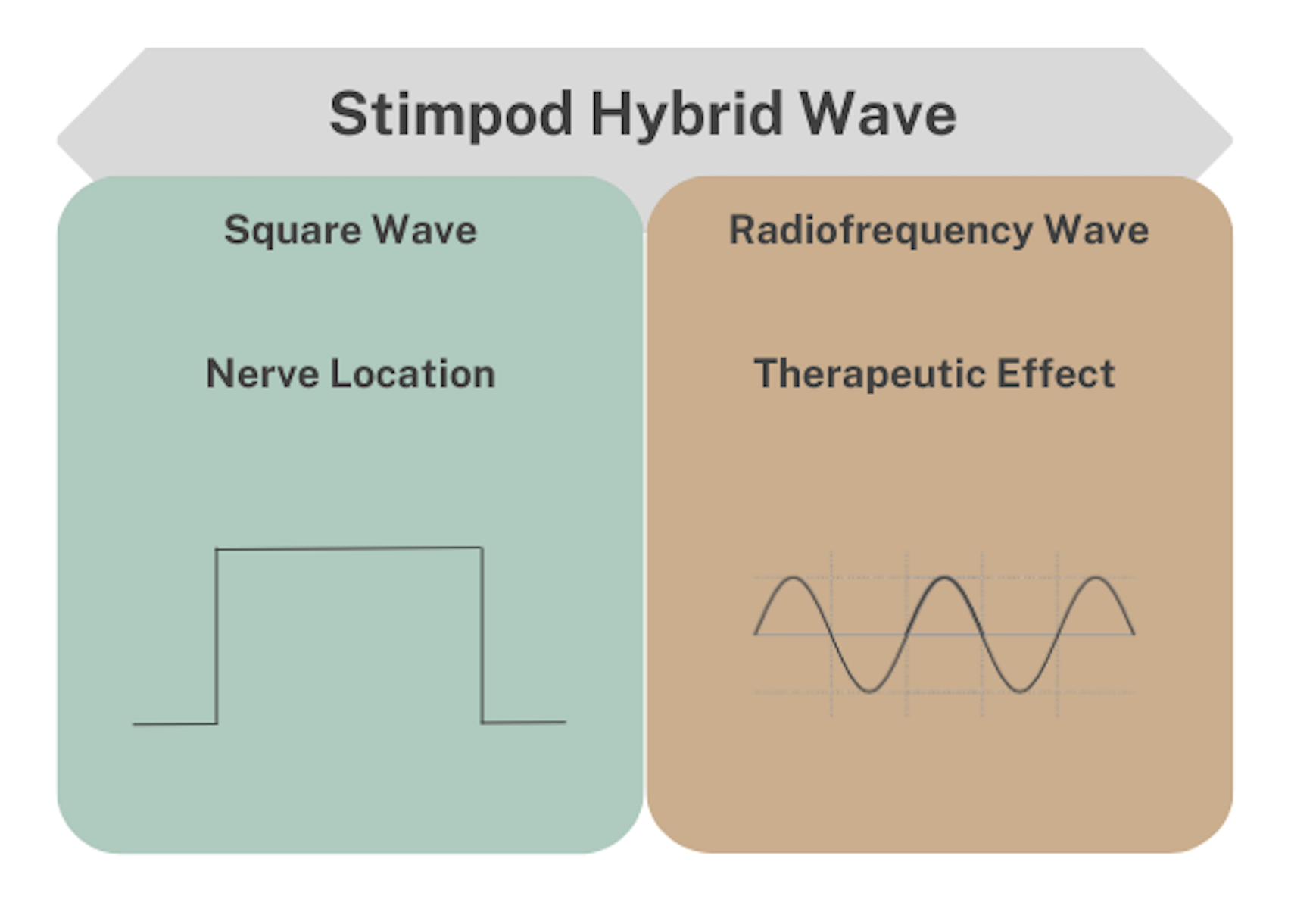
The Stimpod’s therapeutic effect relies on the radiofrequency(+- 100 kHz) component of the hybrid waveform and, without it, there is no significant or no long-lasting therapeutic effect. The Stimpod’s waveform has a fast onset (5 to 10 minutes per nerve) and resets the nerve’s gene expression from a neuropathic state to its original functioning state with no side effects. On the contrary, and as expected, TENS is relatively slow in onset and requires around 30 to 120 minutes of continuous stimulation. Additionally, the pain relief effect disappears quickly once the stimulation is ceased.
In conclusion, Stimpod hybrid waveform takes advantage of the standard square-wave stimulation of any other TENS device, primarily used for nerve location, and adds long-term therapeutic results using the high-frequency component – alleviating pain over a long period (several months) and even permanently in some cases, after only 3-6 short treatments.
