
Diabetic Neuropathy: Current and Emerging Therapeutic Modalities
Worldwide, the number of individuals affected by diabetes reaches 463 million with the vast majority of cases being type 2 diabetes (T2DM). Some of the most common complications of T2DM include cardiovascular disease, kidney disease, foot problem and neuropathy. Peripheral neuropathy is the most common type of diabetic-induced neuropathy, and it is estimated to affect about half of all people with diabetes with significant effects on a person’s quality of life. This type of neuropathy can cause numbness, tingling, and pain in the feet, legs, and hands. In severe cases, it can lead to amputation if it causes complications such as foot ulcers or infections.
Diabetic neuropathy is defined as a dysfunction of peripheral nerves, following a distal-to-proximal progression, and manifesting through symptoms and signs of pain and/or sensitization, muscle weakness, and numbness or desensitization. The exact cause of diabetic neuropathy is not fully understood, but it is believed to be related to high blood sugar levels.
Objective diagnosis of diabetic neuropathy can be performed with electrophysiological testing which measures nerve conduction velocities (NVC) of large nerve fibers. NVCs are a useful tool for detecting damage to motor nerves, which are responsible for controlling muscle movement. However, they are not as effective at detecting damage to sensory nerves, which are responsible for carrying sensory information such as touch, and pain from the body to the brain. To assess sensory nerve damage, healthcare providers may use other diagnostic tools such as quantitative sensory testing (QST) or questionnaires such as the Douleur Neuropathique en 4 (DN4).
Diabetic neuropathy can be difficult to treat, and, to this day, it is still considered an irreversible disease with no cure. However, there are a number of things that people with diabetes can do to reduce their risk of developing neuropathy or to manage the condition if they have it.
First and foremost, it is important for people with diabetes to carefully manage their blood sugar levels. This can help to prevent or delay the onset of neuropathy. It is also important to eat a healthy diet, exercise regularly, and avoid smoking and excessive alcohol consumption.
For those who already have diabetic neuropathy, there are a number of treatments available to help manage the condition. These can include medications to control pain and other symptoms, physical therapy to improve mobility and strength, and specialized shoes or inserts to protect the feet in case of ulcers or infections or to help with mobility.
Current standard of care for diabetic neuropathy include:
- Medications: There are several medications that can help to control pain and other symptoms of neuropathy. These can include pain relievers, antidepressants, and anticonvulsants.
- Physical therapy: Exercise and other forms of physical therapy can help to improve mobility and strength in people with neuropathy.
- Orthotic devices: Specialized shoes or inserts can help to protect the feet and reduce the risk of foot injuries.
Emerging technologies for diabetic neuropathy include the use of electromagnetic therapies which leverage on the interaction between electromagnetic fields and biological systems. Devices like the STIMPOD NMS460 (Algiamed Technologies) can stimulate affected nerves and induce long-term pain relief, as demonstrated in recent clinical trials on patients with pedal diabetic neuropathies.
PEMF therapy involves the application of electromagnetic fields to the body using specialized devices. It is a non-invasive, non-pharmacological approach that can be administered using various devices, such as mats, pads, or specialized machines. These devices generate electromagnetic pulses that penetrate the body and potentially affect various cellular and molecular processes. The therapy aims to stimulate cellular repair, improve blood flow, reduce inflammation, and modulate pain perception.
The potential benefits of PEMF therapy include:
- Enhanced tissue healing and regeneration.
- Reduction of pain and inflammation.
- Improved circulation and oxygenation of tissues.
- Enhanced bone healing and fracture repair.
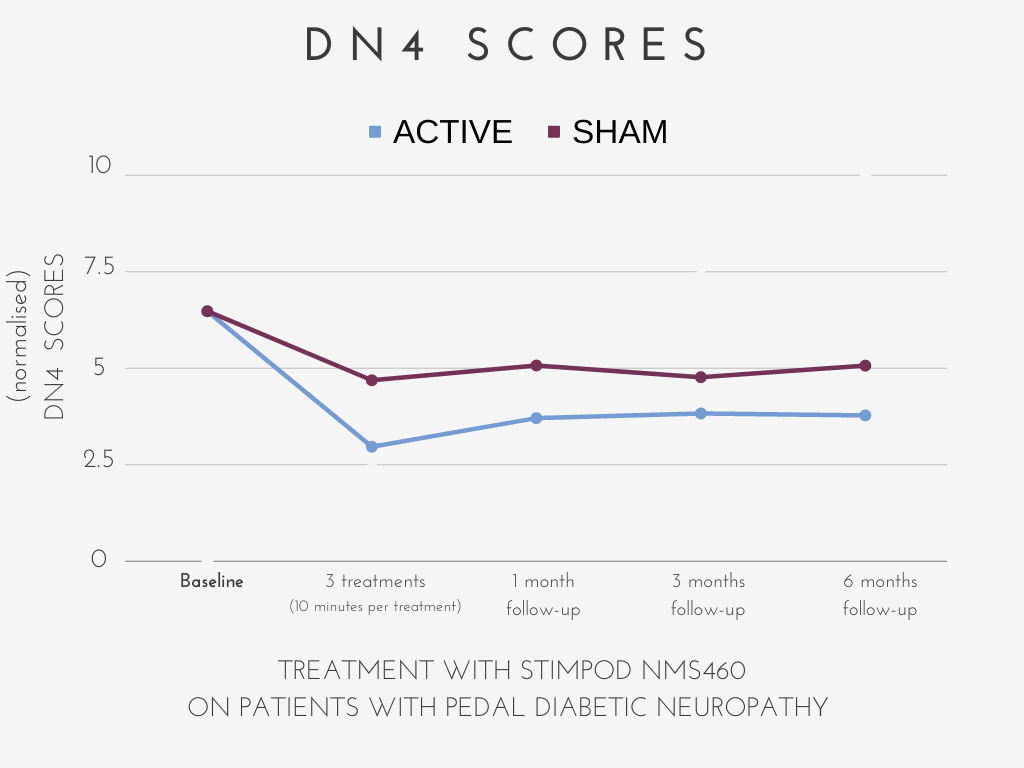
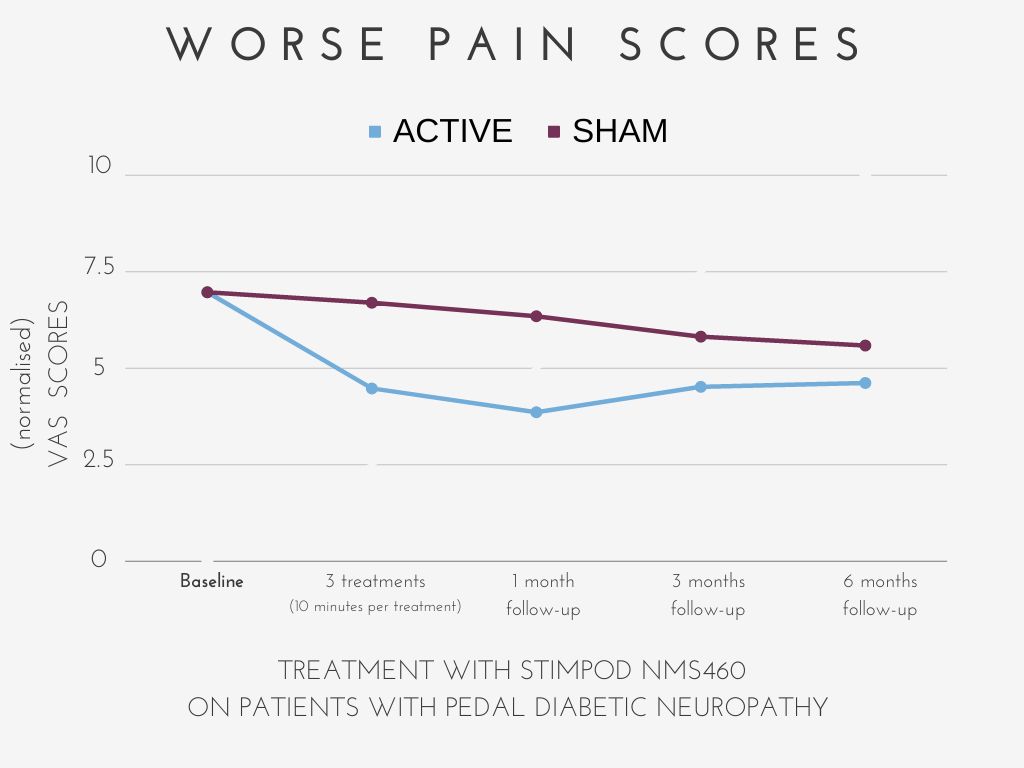
Figure 1 – (left) the DN4 test demonstrates significant improvement in neuropathic pain symptoms in patients receiving active treatment with STIMPOD NMS460. (right) likewise, VAS scores for worse experienced pain demonstrate a significant reduction after 3 treatments with STIMPOD NMS460. Results remained significantly reduced even 6 months after the last treatment suggesting long-term therapeutic efficacy.
Read more about this at:
- “Can an electrical pulsed radio frequency device relieve pain and improve function in patients with pedal diabetic neuropathy? A single blind randomized placebo-controlled trial.” by P. Berger and S. Landau, 2016
https://restorativespot.com/wp-content/uploads/2020/12/PAINSA-PRF-diabetic-neuropathy.pdf
In conclusion, diabetic neuropathy is a serious complication of diabetes that can have significant impacts on a person’s quality of life. While there is still no cure available, careful management of blood sugar levels and other lifestyle factors can help to prevent or delay the onset of neuropathy, and there are treatments available to manage the condition if it does occur.
Figure 1 – (up) the DN4 test demonstrates significant improvement in neuropathic pain symptoms in patients receiving active treatment with STIMPOD NMS460. (bottom) likewise, VAS scores for worse experienced pain demonstrate a significant reduction after 3 treatments with STIMPOD NMS460. Results remained significantly reduced even 6 months after the last treatment suggesting long-term therapeutic efficacy.
Read more about this at:
- “Can an electrical pulsed radio frequency device relieve pain and improve function in patients with pedal diabetic neuropathy? A single blind randomized placebo-controlled trial.” by P. Berger and S. Landau, 2016
https://restorativespot.com/wp-content/uploads/2020/12/PAINSA-PRF-diabetic-neuropathy.pdf
In conclusion, diabetic neuropathy is a serious complication of diabetes that can have significant impacts on a person’s quality of life. While there is still no cure available, careful management of blood sugar levels and other lifestyle factors can help to prevent or delay the onset of neuropathy, and there are treatments available to manage the condition if it does occur.
